Lymphedema
Localized fluid accumulation
Lymphedema is a condition in which an abnormal amount of fluid and proteins accumulates in a body part. There is an imbalance between the supply and removal of this fluid.

Lymphedema can be caused by a congenital defect or, for example, by an illness, operation or medication. Both forms can lead to serious physical symptoms.
Description of condition
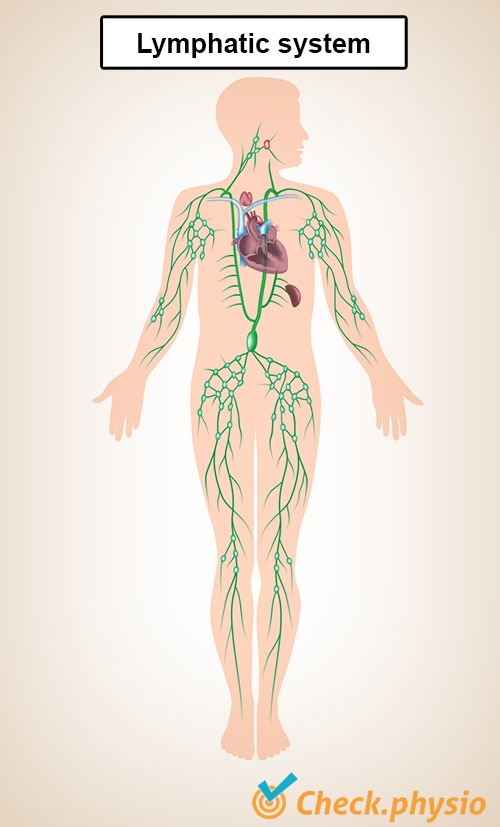
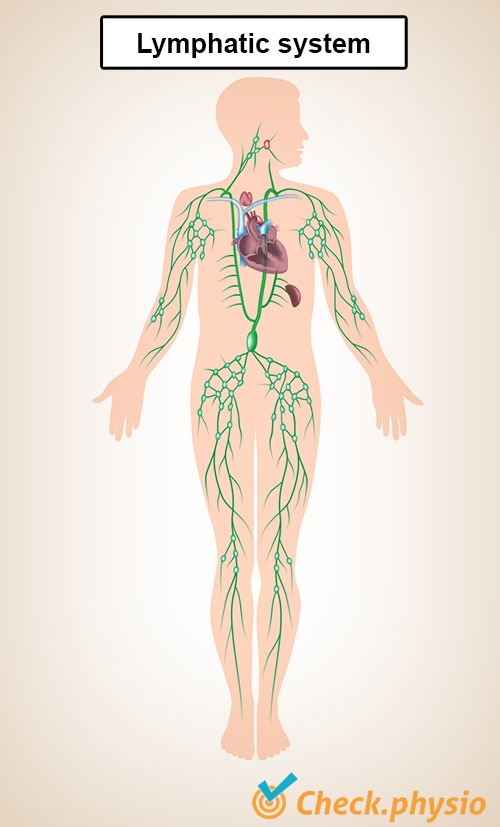
Lymph vessels and lymphatic pathways are found throughout the body. These end in the lymph nodes. Groups of these lymph nodes can be found, for example, in the groin, armpit, neck and abdomen.
The task of the lymphatic system is to transport and purify the lymph fluid, which is then released back into the bloodstream. The lymphatic system helps remove fluid and waste products and fight infections. When this system does not work properly, an accumulation of fluid, the lymphedema develops.
Cause and history
Lymphedema can be divided into two types: congenital and acquired lymphedema. In case of congenital lymphedema, there is a defect in the lymphatic system that takes care of the supply and drainage of lymph fluid.
There may not be enough lymphatic vessels present or they are too narrow or, on the other hand, too wide. Problems also arise when the lymph nodes do not function properly. When the abnormalities are serious, symptoms may already be present from birth. The symptoms are then usually present in (both) feet and legs.
The lymphedema may also spread to other parts of the body such as the arms and the face. In milder cases, symptoms usually arise between the age of 18 and 35 and are then more usually present on one side. Women are four times more likely to develop lymphedema, partly due to hormonal changes, the monthly hormonal cycle and possible pregnancy(ies).
Non-congenital or acquired lymphedema can occur for instance after surgery, radiotherapy, infection, use of medication or as a result of a trauma which damages the lymphatic vessels or nodes.
Lymphedema is seen relatively often in people who are treated for cancer. This may include the removal or irradiation of part of the lymph nodes. This causes damage to the lymphatic system so that it no longer functions properly. Tumors, too, can compress the lymphatic vessels.
Most forms of lymphedema are not hereditary, certainly not the acquired variety. However, there may be a familial predisposition.
Signs & symptoms
People who suffer from lymphedema may experience varying levels of symptoms such as:
- Swelling of one or more body parts.
- Pain and/or tingling.
- Local fatigue and a heavy feeling in the affected area.
- Restrictions in movement due to swelling and/or pain.
- Skin abnormalities such as fluid-filled blisters, hardening of the skin, blue spots or nodules.
- Infections.
Diagnosis
To find out if it is lymphedema, the doctor will ask a number of questions about the symptoms. It is important to find out whether there has been surgery or trauma, for example, or whether there is a disease that could explain the swelling.
In case of congenital lymphedema, the doctor will also ask if there are other people in the family with these symptoms. In addition, a physical examination will be performed including an examination of the affected body part.
Swelling is the most pronounced symptom of lymphedema. This swelling can be divided into pitting and non-pitting edema and can be tested using the Godet test. When pressing on the swelling with a finger, a small impression may remain visible for a short period of time, this is called pitting edema. When the swelling is hard and cannot be easily pressed, this is called non-pitting edema. When the lymphedema has been present for a long time, the tissue hardens so that it can no longer be compressed. In this way, the Godet test can be used to work out the stage of the lymphedema.
In addition, doctors use the Stemmer maneuver. This is to check if changes are present in the skin between the second and third toe or finger. When the skin cannot be lifted at this spot, this is an indication for lymphedema.
In rare cases, additional testing, called lymphoscintigraphy, is performed. This procedure maps out how the lymph fluid is draining and where possible obstructions are located.
Treatment
A specially trained physiotherapist, an edema therapist, plays an important role in the treatment of lymphedema. Within the treatment of lymphedema, two phases can be distinguished. These are the reductive phase and the maintenance phase.
The reductive phase is aimed at reducing the lymphedema as quickly as possible. This is done, among other things, through lymphatic drainage in which the edema therapist applies a specific massage technique. The edema therapist may also use a special taping technique with elastic tape to stimulate the drainage of lymph fluid.
Exercise is also a good way of effectively pumping the fluid away by contracting and relaxing the muscles. In addition, it may be necessary to wear bandages or support stockings to prevent the swelling from returning (quickly). As long as an improvement is obtained, these techniques can continue to be used intensively.
If there is no further improvement, the treatment will move on to the maintenance phase. In this phase, the aim is to keep the symptoms under control. In principle, the treatment is the same as in the reductive phase, only the frequency of treatment decreases. Lymphedema is a chronic disorder that requires lifelong treatment.
Sometimes the above treatment is not sufficient and it is necessary to intervene with surgery. In this case, fluid, connective tissue and fatty tissue are removed. Even after this operation, treatment by an edema therapist is necessary.
Exercises
You can check your symptoms using the online physiotherapy check or make an appointment with a physiotherapy practice in your locality.
References
Damstra, R.J. (2014). Richtlijn lymfoedeem. Multidisciplinaire evidence-based richtlijn. Utrecht: Nederlandse Vereniging voor Dermatologie en Venereologie.